Effects of COVID-19 pandemic on mental health have a lasting effect on their overall well-being. This may vary from a panic behaviour or collective hysteria to pervasive feelings of hopelessness and desperation with negative outcomes including suicidal behavior.


The current situation is causing mental health problems such as stress, anxiety, depressive symptoms, insomnia, denial, anger and fear. The main aim of research is to study the effect of mental health due to covid-19 pandemic. These mental health problems not only affect attention, understanding and decision-making capacity of medical workers, which could hinder the fight against COVID-19, but they could also have a lasting effect on their overall well-being .
The psychological reactions to COVID-19 pandemic on population may vary from a panic behavior or collective hysteria to pervasive feelings of hopelessness and desperation which are associated with negative outcomes including suicidal behavior. Importantly, other health measures may be compromised by abnormally elevated anxiety.
Method:
This paper aims to review the latest papers referring to the effect of pandemic on mental health by using an online questionnaire method. A survey was conducted through a google form link shared on various social media . It was conducted from 19 september 2020 to 24 September 2020. The population of the world who agreed to participate in study were included by a simple random method . Populations aged 18 years or more were included in this survey .
Study Tools:
Then the set of several questions will appear consecutively in which the participants will answer. This study was conducted among 301 people in the world and response came from India ,USA , London , Canada, Australia and Kenya. Out of them ,
255 (84.71%) people were from India, 26 (8.6%) people were from the USA, 10 (3.32%) people were from Canada, 5 (1.66%) people were from Australia, 3 (0.99%) people were from London, and 2 (0.66%) people were from Kenya. Out of 301 participants , 152 (50.49%) were male and 149 (49.5%) were female.
Age
Total 12 questions were conducted in an online survey and options were based on everyday , very often , sometimes and not at all .
The covid-19 pandemic is by definition, a significant threat to humanity. The pandemic is straining our healthcare and economic system in ways that are significant and obvious .
Following psychological signs are observed :
Uncontrollable fear
This is commonly one of the most frequent psychological reaction to pandemics. Several existing studies demonstrated that those who have been exposed to the risk of infection may develop pervasive fears about their health, worries to infect others and fear infecting family members.
Frustration and irritation
Distress, boredom, social isolation and frustration are directly related to confinement, abnormally reduced social/physical contact with others, and loss of usual habits. As per report frustration and pervasive irritation seem to derive from the inhibition from daily activities, interruption of social necessities, not taking part in social networking activities.
Loneliness
Pervasive loneliness may be significantly associated with increased depression and suicidal behavior.Pervasive loneliness may be significantly associated with increased depression and suicidal behavior.
Insomnia
Due to stressful life, impaired sleep and circadian rhythms at a time when healthy sleep is particularly important to cope adaptively with this crisis uncertainty about the future.
The above symptoms if left untreated can result into various chronic mental disorders :
1) Schizophrenia :
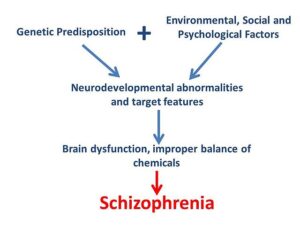
While there is no cure for schizophrenia, research is leading to innovative and safer treatments. Experts also are unraveling the causes of the disease by studying genetics, conducting behavioral research, and using advanced imaging to look at the brain’s structure and function. These approaches hold the promise of new, and more effective therapies.
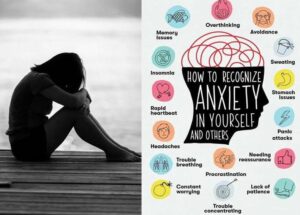
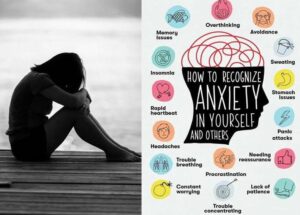
2) Anxiety :
Everyone feels anxious now and then.Occasional anxiety is OK. But anxiety disorders are different. They are a group of mental illnesses that cause constant and overwhelming anxiety and fear. The excessive anxiety can make you avoid work, school, family get-togethers, and other social situations that might trigger or worsen your symptoms.
Types of Anxiety disorders
There are several types of anxiety disorders:
- Generalized anxiety disorder
- Panic disorder
- Specific phobias
- Separation anxiety
- Medication-induced anxiety disorder
3) Depression
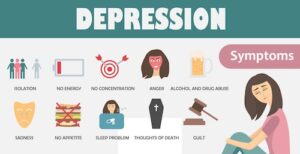
Depression (major depressive disorder) is a common and serious medical illness that negatively affects how you feel, the way you think and how you act. Fortunately, it is also treatable. Depression causes feelings of sadness and/or a loss of interest in activities once enjoyed. It can lead to a variety of emotional and physical problems and can decrease a person’s ability to function at work and at home.
Depression symptoms can vary from mild to severe and can include:
- Feeling sad or having a depressed mood
- Loss of interest or pleasure in activities once enjoyed
- Changes in appetite — weight loss or gain unrelated to dieting
- Trouble sleeping or sleeping too much
- Loss of energy or increased fatigue
- Increase in purposeless physical activity (e.g., hand-wringing or pacing) or slowed movements and speech (actions observable by others)
- Feeling worthless or guilty
- Difficulty thinking, concentrating or making decisions
- Thoughts of death or suicide
Symptoms must last at least two weeks for a diagnosis of depression.
4) Bipolar disorder :
Bipolar disorders are brain disorders that cause changes in a person’s mood, energy and ability to function. Bipolar disorder is a category that includes three different conditions — bipolar I, bipolar II and cyclothymic disorder.
People with bipolar disorders have extreme and intense emotional states that occur at distinct times, called mood episodes. These mood episodes are categorized as manic, hypomanic or depressive. People with bipolar disorders generally have periods of normal mood as well. Bipolar disorders can be treated, and people with these illnesses can lead full and productive lives.
Psychological approaches


Psychiatrists can play an essential role in supporting the well-being of those affected and their families and crucial interventions can be related with the education about the common adverse psychological costs and encouraging health-promoting behaviours, the facilitation of problem solving and finally the empowerment of the patients, their families and health-care providers.
Characteristics of studies reporting psychological parameters
| Region of university | Author | Year of publication | Type of paper | Sample size |
| Rollins School of Public Health, Emory University, Atlanta, Georgia, USA | Druss BG | 2020 | Viewpoint | 0 |
| Department of Psychiatry, National Institute of Mental Health and Neurosciences (NIMHANS), Hosur Road, Bangalore 560029, India | Banerjee D | 2020 | Letter | 0 |
| School of Epidemiology and Public Health, Child and Adolescent Psychiatry, University of Ottawa, Ottawa, Ontario, Canada | Gardner W | 2020 | Viewpoint | 0 |
| Neurology and Physical Medicine and Rehabilitation and Chief of Pain Medicine, Johns Hopkins School of Medicine, USA | Cohen S | 2020 | Recommendation and guidelines | 0 |
| Metro South Addiction and Mental Health Service, Brisbane, Australia | Dan Siskind | 2020 | Paper for clinician with recommendations | 0 |
| Centre for Behavioural Science and Applied Psychology, Sheffield Hallam University, UK | Arden MA | 2020 | Letter | 0 |
Psychological Impact On Other Countries
In the USA, the crisis has highlighted the extent of interconnectedness of their institutions, including medical, public health, political, economic, and educational. The current pandemic clearly underscores the global nature of their lives today and the limited constructs of nationality, religion, and political leanings in the face of a common threat. They cannot fully anticipate the long-lasting effects of this pandemic on our societies.
There they have seen telemedicine set up at record speed to meet the needs of patients. Regulatory barriers to reach many patients were brought down almost overnight. They can use more platforms and cross state lines to deliver care, which are important changes that help us reach as many patients as possible. They are collectively experiencing a stressor that affects segments of the population in different ways.
Pandemia and social psychiatry
Result of the survey:
From above survey , following result have been obtained:
1. There are 22% of people who daily suffer from uncontrolled fear due to covid-19. 53% have sometimes fear of covid -19.
2. There are 50% people who are daily concerned about their and their family’s health and safety.
3. There were less changes found in the sleep pattern of people due to this covid-19 pandemic.
4. Less than 75% of people are losing their interest in the academic activities.
5. As 18-25 years participants were more so there were 34% not applicable for this category and rest people sometimes were concerned about their financial condition.
6. From the above graph less than 60% people suffer from loneliness and frustration.
7. There were more than 60% people who got angry on small things due to the pandemic conditions.
8. From the survey we concluded that there was a mild change in appetite of people.
9. There were 70% people scared due to watching news and reading newspapers regarding covid information.
10. Due to covid-19 we have found that more than 60% people suffered from lack of concentration.
11. 9% of people were having suicidal thoughts which should be taken care of and work for it as soon as possible.
Conclusion
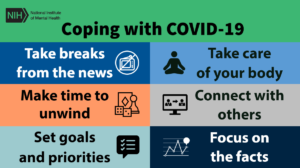
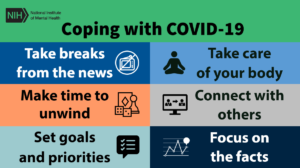
From this survey we found that there is a mild to moderate effect on mental health due to covid-19 pandemic. Implementing community-based strategies to support resilience and psychologically vulnerable individuals during the COVID-19 crisis is fundamental for any community. To cope up with covid-19 pandemic people are trying best to take care of mental health by thinking positive, accepting current situation and doing meditation.
Even they are trying to keep in touch with friends and relatives , taking care of family and keeping busy with different activities.The psychological impact of fear and anxiety induced by the rapid spread of pandemic needs to be clearly recognized as a public health priority for both authorities and policy makers who should rapidly adopt clear behavioral strategies to reduce the burden of disease and the dramatic mental health consequences of this outbreak.


Krishani Patel-(L)
2nd year MBBS student
AMCMET medical college , ahmedabad
Vishani Patel-(R)
3rd year MBBS student
GMERS Medical college, Patan.
References
1 WHO. Coronavirus disease (COVID-19) pandemic. WHO emergencies (Internet). Geneva, Switherzland, Updated 6 Mar 2020 Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
2 WHO. Coronavirus disease 2019 (COVID-19) Situation Report-70 (Internet). Geneva, Switherland, Updated 19-30 March 2020. https://www.who.int/publications-detail/covid-19-operational-guidance-formaintaining-essential-health-services-during-an-outbreak.
3 Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry 2020;63:e32.
4 Duan L , Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry 2020; 7:300–2.
5 Barbisch D , Koenig KL, Shih FY. Is there a case for quarantine? Perspectives from to Ebola. Disaster Med Public Health Prep 2015 ; 9 :547–53.
6 Rubin GJ, Wessely S. Coronavirus: the psychological effects of quarantining a city. BMJ Opinion 2020; 368:m313.
7 Jones, N. M., Thompson, R. R., Dunkel Schetter, C., Silver, R. C. (2017). Distress and rumor exposure on social media during a campus lockdown. Proceedings of the National Academy of Sciences of the United States of America, 114, 11663–11668. https://doi.org/10.1073/pnas.1708518114
8 Kang, L., Li, Y., Hu, S., Chen, M., Yang, C., Yang, B. (2020). The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. The Lancet Psychiatry, 7, E14.
9 The outbreak ofCOVID-19 coronavirus and its impact on global mental health
https://doi.org/10.1177/0020764020915212
10 Druss BG. Addressing the COVID-19 pandemic in populations with serious mental illness. JAMA Psychiatry 2020 [Epub Ahead of Print].
11 Banerjee D. The COVID-19 outbreak: cucial role the psychiatrists can play. Asian J Psychiatr 2020;50:102014.
12 Freeman MP. COVID-19 from a psychiatry perspective: meeting the challenges. J Clin Psychiatry 2020;81:20ed13358.
13 Bai Y , Lin C-C , Lin C-Y , Chen J-Y , Chue C-M , Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv 2004; 55:1055–7.
14 Reynolds DL , Garay JR , Deamond SL , Moran MK , Gold W , Styra R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol Infect 2008; 136:997–1007.
15 Hawryluck L , Gold WL , Robinson S , Pogorski S , Galea S , Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis 2004; 10:1206–12.
16 DiGiovanni C , Conley J , Chiu D , Zaborski J. Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecur Bioterror 2004; 2:265–72.
17 Cava MA , Fay KE , Beanlands HJ , McCay EA , Wignall R. The experience of quarantine for individuals affected by SARS in Toronto. Public Health Nurs 2005; 22:398–406.
18 Jeong H , Yim HW , Song Y-J , Ki M , Min JA , Cho J , et al. Mental health status of people isolated due to Middle East respiratory syndrome. Epidemiol Health 2016; 38:e2016048.
19 Desclaux A , Badji D , Ndione AG , Sow K. Accepted monitoring or endured quarantine? Ebola contacts’ perceptions in Senegal. Soc Sci Med 2017; 178:38–45.
20 Braunack-Mayer A , Tooher R , Collins JE , Street JM , Marshall H. Understanding the school community’s response to school closures during the H1N1 2009 influenza pandemic. BMC Public Health 2013; 13:344.
21 Amerio A , Bianchi D , Santi F , Costantini L , Odone A , Signorelli C , et al. Covid-19 pandemic impact on mental health: a web-based cross-sectional survey on a sample of Italian general practitioners. Acta Biomed 2020; 91:83–8.