Thalassemia Care in India: Where do we stand? In India it is estimated that 10,000 to 12,000 children are added every year to the pool of Thalassemia patients. So the disease needs immediate attention.
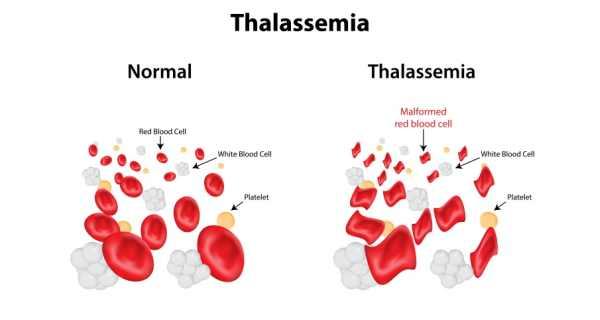
Blood, the life line of our bodies, has three major cellular components: red cells, white cells and platelets. Red cells provide energy and transport oxygen in the body. In Thalassemia major, red cells synthesis is insufficient and the life span also is very short. The disease manifests early in childhood, mostly in the first year of life, and these patients require lifelong frequent blood transfusions (every few weeks) to keep them alive.
Burden of the problem: – 80% of the children with this disease are born in Asian Subcontinent and the Middle Eastern countries. In India it is estimated that 10,000 to 12,000 children are added every year to the pool. Parents, usually asymptomatic are the carriers of this disease and there is 25% risk of this disease affecting their children. The carrier state in Indian population varies from < 1% to up to 17% in some ethnic communities, with an average of 3.3%. So the disease burden is significant and worth immediate attention.
Challenges with blood transfusion: – Needless to say that these patients need timely supply of safe blood. It has been estimated that annual requirement of packed red cells is about 2 million units in India. Although patient organizations, Indian Red Cross Society and other regional blood banks have been working relentlessly towards fulfilling this requirement, but the demand is significantly more than the supply. Lot of families have to struggle month after month in making packed cells available for their children. In a country of 1.2 billion people, can we pledge today that we donate blood to save precious lives of thousands of thalassemic children.
As blood is potential medium for transmission of infection, it is very important that blood these patients receive in safe. Although Government of India under NACO programme makes it mandatory to test for blood transmitted disease like syphilis, hepatitis B, hepatitis C and HIV, this is still not universally practiced, especially in smaller town. Even testing for these infections by traditional methods leaves some children at risk, if blood is collected in “window period”. Newer methods like NAT testing should be made compulsory and sponsored to minimize the risk of infection transmission in this window period.
Iron chelation: Repeated packed cell transfusions lead to iron overload, which deposits in important organs like liver, heart and endocrine glands. This iron overload is usually the cause of death in the second or third decade of life. These patients need to be on medications to remove this extra iron from the bodies and if adequately chelated, they can have normal life span. Inspite of freely available drugs, less than 10% of the patients are adequately chelated. Various factors like ignorance, poor compliance and more importantly unaffordability are major reasons for poor chelation. Very few state governments have made these drugs available to the patients, but supplies are erratic and inadequate. There is need of a central legislation making these drugs available freely and free of cost to these patients.
Centres for care of thalassemics: Thalassemia is a multi system problem and in addition to packed cell and iron chelation, need management by a multidisciplinary team. This team should have hematologist, endocrinologist, cardiologist, nutritionist, nurse practioner etc. for holistic care of these patients. There are hardly if any comprehensive centres for thalassemia care and a rough estimate is that <5% thalassemia patients receive care in such centres. There is an urgent need for having such regional centres which can coordinate and monitor thalassemia care.
Bone marrow transplantation:- Bone marrow transplantation is currently the only curative option available for this condition. Recent data shows more than 90% success rate of bone marrow transplantation in patients who have HLA matched siblings. Very very small percentage of cases undergoes this procedure. Factors like ignorance about the procedure, affordability and inadequate centres where this treatment is available, are some obstacles towards this curative treatment. There is a need of government organizations, non-government organizations and other leaders to come together and support this curative treatment programme.
Preventive measures: Need of the hour is to have an efficient, countrywide programme for prevention of thalassemia, as the magnitude of problem both economic and social in huge. Screening for thalassemia carriers, needs to be made compulsory and antenatal testing made freely available in order to detect the disease very early in pregnancy. If small countries like Cyprus have been able to eliminate this problem by efficient national thalassemia prevention programme, why can’t we?
Need for patient Advocacy groups: Best advocates for change and improvement can be patients / families themselves. Thalassemia societies in some states have catalysed a tremendous change in the Thalassemia care by virtue of constant advocacy. There is a need for these patient / family groups to be formed in each city / state. These advocacy groups can identify the problem areas and bring them in the notice of the political establishment.
In summary, the magnitude of the problem of thalassemia is huge, but unfortunately inadequately addressed. There is a need for the Ministry of Health to put it on the “priority list” and address to the issues, which are numerous. There is also a need for the medical experts and the families to get together and be advocates for their patients. With these collaborative efforts, our thalassemic children shall also get the standard care which they deserve!

Dr. Sunil Bhat
Senior Consultant & Head Pediatric Hematology, Oncology and Blood & Marrow Transplantation
Mazumdar Shaw Cancer Centre, Narayana Health City Bangalore, India