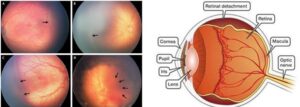
Retinopathy of Prematurity or ROP is defined as a disorder of the developing retina of low birth weight, preterm infants potentially leading to blindness in a small but significant percentage of those infants.
ROP is not a new disease but the number of babies at risk for ROP is increasing because of the improvement in neonatal care and better practices in NICU. As such the management of babies with ROP is a combined effort of neonatologists, ophthalmologists and a host of other health care personnel. Accordingly the theme for the World prematurity day 2020 which falls on 17th November is “Together for babies born too soon – Caring for the future”
Which babies are at risk for ROP?
There are many guidelines with regard to ROP. The guidelines stated below are best suited for Indian babies
- Children born with birth weight less than 2000 grams·
- Children born before gestational age of 34 weeks·
- Children who have been exposed to oxygen for more than 30 days
Other factors where screening must be done for children with birth weight <2000 grams or Gestational age < 37 weeks include·
- Respiratory distress syndrome·
- Multiple blood transfusions·
- Infection·
- Apnoeic episodes·
- Multiple births·
- Intraventricular haemorrhage·
- Any other case where the paediatrician has concerns
When to screen for ROP?
All children must be screened at least once by 31 weeks gestational age or 3-4 weeks after birth (whichever is earlier)
If the baby has a birth weight < 1200grams or is born before 24 weeks gestational age, examination must be scheduled at 2- 3 weeks post-delivery.
There is no need for examination within 2 weeks of delivery as the normal retinal maturation would not be completed
Preparation for examination:
The baby must be dilated using half diluted commercially available tropicamide- phenylephrine combination. Recently, some companies have come out with ready to use drops where the constituent drugs have been diluted to levels which are deemed safe for the babies. 2-3 instillations of drops are applied 5 minutes apart and examination must be done after 30 to 45 minutes. Any excess drops on cheek must be immediately wiped off to prevent systemic absorption.
What happens after the examination?
The eye specialist examining the baby would advise based on the findings inside the eye. The following outcomes would be possible
- Retina is fully matured – Baby will need a follow up after 6 months or 1 year
- Retina is immature but there is no ROP – Baby will need close follow up
- ROP is present but is not severe – Baby will need close follow up
- ROP is present and severe – Baby will need LASER / intraocular injections /surgery in any possible combination
Can we delay the LASER / Surgery as the baby is small?
Surgery/LASER cannot be delayed as ROP is a rapidly progressing condition and any delay might only end up causing the condition to worsen, however, both LASER and surgery would be conducted under strict monitoring keeping in mind the fragile state of the baby and hence will not affect the baby adversely.
Will the baby recover after the LASER/Surgery?
ROP is the manifestation of the baby’s systemic condition in the eye. Recovery after LASER/Surgery would depend upon how quickly the systemic condition stabilizes.
Will the baby have good vision after LASER/Surgery?
If intervention is done in the early stages of ROP, when the central part of the retina is not yet affected, vision is usually not affected. In the long term, the baby might need to use some glasses in the future but they will enjoy good vision with the same. If the ROP is severe or affects the central part of the eye, the visual outcome might be lesser.
However, one must remember that without any intervention, the child might have gone completely blind. So, in a nut shell all the babies at risk must be examined and those babies needing LASER/surgery must be treated at the earliest to get the best results for the baby.
Also Read: Beat-the-eye-strain-with-healthy-robust-food

Dr Tandava Krishnan
Vitreo retinal surgeon
Maxivision super specialty Eye Hospital
Hyderabad