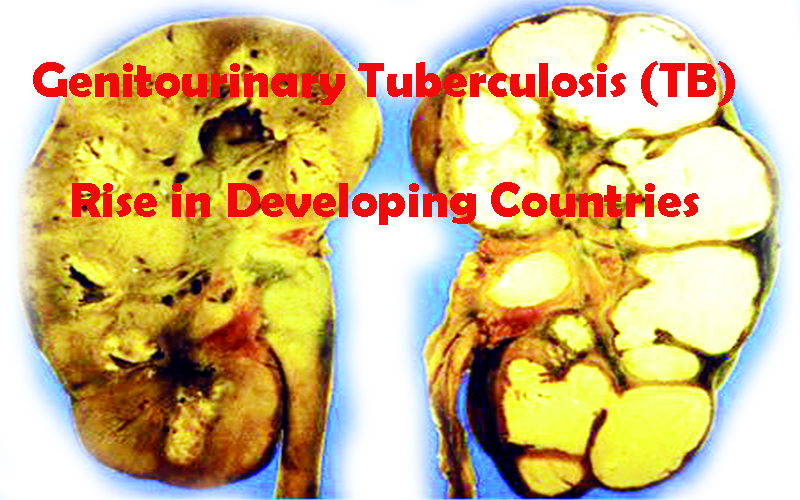
Genitourinary Tuberculosis (TB) on the Rise in Developing Countries, with Devastating Consequences for Reproductive Health
Genitourinary Tuberculosis (TB) is a major public health challenge in developing countries like India, where 14 million people are affected, especially those in the reproductive age group. The incidence of genital TB is on the rise, partly due to its association with human immunodeficiency virus infection. The clinical presentation of genital TB is protean, and it can also be completely asymptomatic.
The disease is most commonly asymptomatic or presents with infertility as the most common symptom, as well as menstrual irregularities, pelvic pain, abnormal vaginal discharge, and other related symptoms. Diagnosis of the disease is challenging, as it requires detection of acid-fast bacilli on microscopy or culture on endometrial biopsy, histopathological detection of epithelioid granuloma on biopsy, and other diagnostic techniques.
The treatment of genital TB is a long and challenging process, and requires daily therapy of rifampicin, isoniazid, pyrazinamide, and ethambutol for 2 months, followed by daily 4-month therapy of rifampicin and isoniazid. Alternatively, a 2-month intensive phase of RHZE can be daily followed by an alternate-day combination phase (RH) of 4 months. Surgery is rarely required, only as drainage of abscesses.
Genital TB can lead to serious damage to the reproductive organs leading to infertility and subsequent sterility. It is responsible for 1% of all gynecological admissions in India and 17.4% in infertility clinics. The prevalence of genital TB in India is reported to be 18%–19% among infertile women and is highly variable. The causes for infertility can be ovulation issues, tuboperitoneal issues, endometrial issues, inflammation, fibrosis, atrophy, toxins, mechanical obstruction, and inflammatory mediators.
The aim of the investigations is to confirm the diagnosis and assess the activity of the disease. After arriving at a diagnosis, all cases should be treated with a full course of ATT as incomplete treatment has a high risk of developing drug-resistant TB.
Genital tuberculosis (FGTB) is a significant problem in India, particularly among infertile women. Management decisions for FGTB can be difficult due to the possibility of bacterial infection or previous surgical trauma. However, since the possibility of Koch’s is high and the isolation of MTB is challenging, a course of ATT for 6-8 months should be considered, especially if there is no previous history of pelvic infection, vaginitis, or surgical interference. The bacterium may still be viable within the fibrotic lesion and may get activated later when patient immunity is low.
Reactivation of dormant bacteria can occur during surgical manipulation, such as laparoscopy, hysteroscopy, hysterosalpingography, and pelvic surgery. High-steroid levels and increased vascularity during ovarian stimulation are also thought to be triggering factors in the infertile population undergoing in vitro fertilization (IVF). Empirical use of steroids and immunotherapies in infertile patients with recurrent implantation failure and recurrent pregnancy loss can also increase the risk factor for reactivation.
Interventional procedures such as hysteroscopic adhesiolysis and laparoscopic assessment may be used, but surgical procedures should be avoided due to the risk of complications, including fistulae. Cornual blocks may be treated with cannulation, and ART may be the only option for these women.
While most women with genital TB present with infertility, their prognosis for fertility is poor, even with ATT. The conception rate is low, and live birth rate is still low. IVF with ET may be the only hope for some of these women, with a pregnancy rate of 16.6% per transfer. ART is most successful in genital TB patients, with a 17.3% conception rate, in contrast to only 4.3% with fertility-enhancing surgery.
Since Genital tuberculosis (FGTB) is a widespread issue in India, particularly among infertile women. Early detection and appropriate treatment can lead to successful pregnancies. However, in advanced stages, a careful individualized approach, counseling, and multidisciplinary collaboration are necessary for better results. Assisting patients with ART should be done with caution, as hormonal treatment can cause the disease to reactivate and is counterproductive.
To diagnose FGTB, acid-fast bacilli must be detected on microscopy or culture on endometrial biopsy or epithelioid granuloma on biopsy. Polymerase chain reaction may be false positive and should not be used alone. Laparoscopy and hysteroscopy can identify genital tuberculosis by various findings.
Currently, there is insufficient evidence to support treatment for FGTB in infertile women. The fertility outcome of treated cases is not significantly better than for women who tested positive for DNA PCR but did not receive treatment.
The combination of tuberculosis and pregnancy can have a significant impact on a woman’s physical and mental health. It has been described as a double-edged sword because of the effects of tuberculosis on pregnancy and the newborn’s growth pattern, as well as the effects of pregnancy on tuberculosis progression. Maternal health is affected by the extended debility, a lack of social support, TB complications, nutritional deficiency, and the need for extended anti-TB medications.
Assessment of the damage and its extent is essential to determine the best course of action to improve fertility. With careful management and appropriate treatment, women with FGTB can achieve successful pregnancies.

Dr. Vidya V Bhat
Medical Director
RadhaKrishna Multispecialty Hospital
Girinagar, Bengaluru