Emerging trends of public private partnership – PPP model in Indian healthcare scenario has seen a growing trend.
Public private partnerships or PPP model in healthcare scenario in India has seen a growing trend. The aim of this article is to understand the scope of partnership of private service providers in the public health setup of Indian healthcare. We will begin with understanding the Indian healthcare scenario first.
So what is PPP model?
Snapshot of the Indian healthcare system:
| Stages of healthcare delivery | Provision of services at various stages of healthcare |
| 1. Primary Healthcare | 1. Community care
2.Care for the ones with chronic illnesses. 3. Community outreach programmes such as immunisation. |
| 2. Secondary healthcare | 1. Some specialities such as general physicians, gynae and obs, paediatric care, general surgery are available.
2. These include district hospitals and community health centres. |
| 3. Tertiary Healthcare | 1. Specialised consultative care mostly on referral from primary and secondary level healthcare centres
2. Special ICU’s, advanced diagnostic facilities |
What is the contribution of private and public sectors in Healthcare scenario?
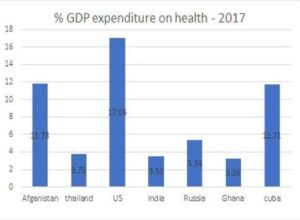
Public health facilities in India consists of sub-centres, primary health centres, secondary health centres and medical colleges and tertiary care centres. These institutions are mostly state or centre government funded. Out of all the spending made for healthcare, only 20% of that is against public healthcare, which is representative of approximately only 1% of the GDP – lowest amongst all the developing and developed countries. As per what is the demand of this country which is the world’s second most populated country, this contribution of public healthcare is negligible.
Demographic changes play a big role in determining the healthcare demands:
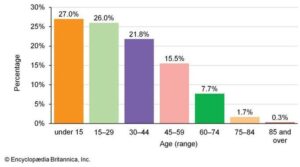
1. Increasing population does not only haunt healthcare but also the existing socio-economic scenario of the country.
2. These changes in demographics come along with altering the disease profiles and increasing the incidence of lifestyle disease like diabetes and cardiac ailments.
3. Urban middle class accounts for the most when it comes to healthcare expenditure. With increase in the population of urban middle class population specifically the demand and consumption of quality healthcare is set to increase.
4. The demand for quality healthcare is also influenced by improved health awareness which comes with increased literacy rates. As the literacy rates are improving the need for above average quality of healthcare is also increasing.
The graph here represents how overall literacy has seen an increasing trend in the past few years.
Does Indian Healthcare infrastructure have enough capacity to fullfill the current healthcare demand?
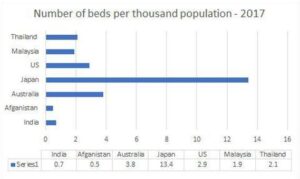
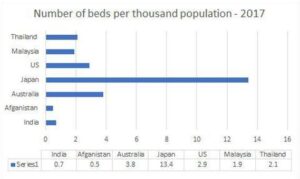
Providing quality healthcare services are highly capital intensive. To build a secondary or a tertiary care hospital it involves no less than 25-40 lakh per installed bed. High manpower requirements ranging from highly skilled doctors to nurses, housekeeping staff, security personnel, lab technicians, front office managers as per the reports and papers published india lackhs in both capital and manpower. India lacks infrastructure so much so that according to 2017 world bank data India has only 0.7 bed per thousand population.
Some states with good economic and healthcare capacity have in excess whereas some performing below the poverty line are too less than the average as described by WHO for the low income countries i.e. 1 bed per 1000 population. To reach the minimum national average, India needs an additional 3 lakh beds. Considering a minimum of 25 lakh per bed cost, an approximate expenditure of 75,000 crore is required in healthcare. In the total healthcare cost maximum expenditure is done on setting up and running of the healthcare unit. Out of the total setting up cost of any hospital 40-65% cost is attributed to land and building.
When national Health Policy 2017 was launched what advisory did it launch?
Key policy principals of NHP-2017 were:
1. Professionalism, integrity, ethics
2. Equity
3. Affordability
4. Universality
5. Patient centered and quality of care
6. Accountability
7. Inclusive partnerships
8. Pluralism
9. Decentralisation
10. Dynamism and adaptiveness
In NHP 2017, government has first time realised the need of private players to collaborate with less expensive public facilities to function to achieve universal health coverage. Govt. also proposes to help private hospitals subsidize costs for people below the poverty line.
If PPP model is implemented, then who will be the stakeholder:
1. Provider
2. Payer
3. Beneficiary
4. Regulator
5. IT infrastructure
Scope of PPP model in India:


2. Purchase and sitribution of drugs in wholesale
3. Contracting out specialists for high risk pregnancy cases
4. National disease control programme
5. Social marketing
6. Adoption and management of PHC’s
7. Medical education and training
8. R&D investments
9. Telemedicine
Key areas where Private players can be involved are:
1. Infrastructure and development
2. Management and operations
3. Capacity building and training
4. Financial mechanism
5. IT infrastructure development for networking and data security
6. Material management
Infrastructure and development:
Planning, designing and development of health infrastructure with innovation and strategy is the area where private partner involvement is done in the case of healthcare infrastructure. Development of infrastructure with innovation could help in bridging the resource gap. Modern healthcare facilities come at a higher price due to high investment costs and hence are still unaffordable for 90% of the population. PPP can offer a solution in this matter by providing land at subsidised costs which reduces a major part of the capital investment during infrastructure development.
Management and operations:
India has a vast health infrastructure but is under utilised due to inadequate management. Ranging from PHC’s to large tertiary health centres, poor management leads to efforts of the government go in vain. To the contrary the private sector has grown exponentially in a short period of time due to right minded management techniques. At PHC level private clinics are performing better than public facilities, due to maybe more facilities, quality of care and better hygiene. Here is where the PPP can intervene by upkeep the infrastructure, maintaining good housekeeping and supply chain, well equipped pharmacy and OPD, well functioning equipment and machineries.
Capacity building and training:
As mentioned above the inadequate management is also due to lack of required skill set in the public facilities. In this case PPP can contribute by providing adequate training to the hospital staff and building their skills set to better utilise the infrastructure and facilities in providing quality healthcare services. Public hospitals are well equipped with space, clinical material for both in-patients and out-patients. With proper training and development of nurses, auxiliary staff and housekeeping staff, these resources can be utilised judiciously. This can be a contractual work which will not require an integrated arrangement for long term, it might be required over some time intervals. Private players can be utilized for continuing education programs for the doctors and nurses.


Dr. Niharika Bansal
International institute of health management and research
Delhi Mob: 995322493