e-PPP model: A way to boost up the rural healthcare system in India. This study suggests that e-PPP model may address the problem of absenteeism and also improve the mode of rural healthcare services.
Effective primary health care is one of the purposes of sustainable development for health care outcome1. The quality of service is the basic concern to access the effective primary healthcare. Qualified doctors and health workers are limited in rural areas of India2. In rural areas health care quality mainly varies due to absenteeism of qualified government MBBS and by their replacement support system through non MBBS workers. Absenteeism of qualified government doctors and nurses is a major drawback of rural health care system.3 Two independent but related issues like weak regulations and lack of financial incentives drive the government doctors to practice in private sectors4. Quality of health care services in highly populated areas is quite important factor for the developing economics to provide effective health care facility.
It has been reported that utilization of government outpatient department (OPD) is only 10 to 20%5. Health care efforts by the practitioner are much better in private clinic than the government OPD6. It has also been stated that the treatment efforts are much poorer in the government sector than private hospitals. It is estimated that in rural areas of north India 45% to 80% unqualified doctors are providing health care services resulting in the substandard services and chances of disease remedy is limited compared to qualified doctor’s treatment7. This study aims to draw attention of policy makers towards regulation and e-public private partnership (e-PPP) to improve rural health care system.
The study is basically brought about by using secondary data obtained from published articles and reports available online. An assessment of various results, facts and reports were contemplated to represent the current scenario of rural health care in India. This analysis was taken to evaluate the opportunities and challenges in the implementation of e-PPP model on rural health care system. The scope of this finding using e-PPP model along with cloud based electronic health record system may help the government to make subtle plans to modulate the rural health care system. Rural health care system reformation and strengthening is one of the purposeful motives for overall booming of health care sector in India.
Demographic indicator in rural health care-Life expectancy is a factor to build up any health care system in the country.In India, life expectancy is 68.56 years according to the data of year 2016. Few states like Kerala, Tamilnadu have 10% more population in 60 years age group. Overall life expectancy rate is more in the rural areas than urban areas8.
Socio-economic indicators in rural health care- Literacy rate determine the level of awareness about healthcare services among people in that particular area. And, the overall literacy rate in rural areas of India is 71%. Kerala (92.98%) and Mizoram (84.10%) have the highest literacy rate in rural areas. On the other hand Bihar has 59.78% of literacy rate in rural areas9.
Critical views on rural health care system in India:
Entire health care system comprises of the government, doctors, nurses, paramedical staff, academicians, health care financer, pharmaceutical companies and health insurance companies etc. Private health care sectors are growing rapidly. But as per the middle class and below poverty line person’s prospective, the accessibility, affordability and availability are the major challenges in India. Public sector of India only spent 1.2 % of GDP, lowest among the other countries10, 11. Rural health care system is three tier system based on facility and average rural population are covered by health care facility depicted in Table 1 and Table 2 respectively12.
| Community Health Centre (CHC) | A 30 bedded Hospital with Specialist services. |
| Primary Health Centre (PHC) | A 4-6 bedded manned with Medical Officer-in-Charge and 14 subordinate paramedical staff |
| Sub-Centre (SC) | Most peripheral point between PHC & CHC manned with one HW(F)/ANM & one HW(M) |
Table 1: Rural health care system in India
| Parameter | Sub Centre (SC) | Primary Health Centre (PHC) | Community Health Centre (CHC) |
| Average population covered by health facility | 5377 | 32884 | 151316 |
| Average rural area (Sq.Km) covered | 20.00 | 122.33 | 562.89 |
| Average radial distance (Km) covered | 2.52 | 6.24 | 13.38 |
| Average number of villages covered | 4 | 25 | 116 |
| * Based on the rural population of 2011 Census | |||
Table 2: Average rural population covered by healthcare facility as on 2016*
According to one WHO report, India is on the 52nd position out of 57 countries facing crisis in human resource of health care division. India is having a huge short fall of general and specialized doctors, but the prominent impacts has been seen in the rural areas as more than 70% population lives in the rural areas12.
e-PPP model in rural health care system- This partnership is basically cooperation between public sector (government) and private sector that fulfill common healthcare goals. e-PPP model in health care system may be defined as a profitable or non profitable initiative. Main aim of this model is to develop a better health care infrastructure, hassle free medical services and treatments regardless of location13, 14. The e-PPP model in health care is depicted in Figure 1.
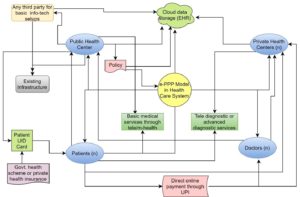
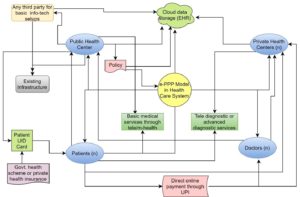
Figure 1: e-PPP model in rural health care
In case of e-PPP model, Public sector provides the existing infrastructure and contract with any third party for info-tech setup in a cost effective manner. Third party must provide effective data security. Public sector establishes the policy of the partnership and data access facility. They also provide online basic health services via tele or m-health approach and national health schemes like Ayushman Bharat or NHPS etc. Any private sector and doctors, as an individual can join this model. It is an open ended model, so no one can establish monopoly or together as oligopoly. Private sectors provide advanced diagnostic services like CT, MRI and better laboratory facility along with advanced medical services via online and offline mode.
All the sectors are linked via cloud based electronic health record (EHR) and unique id (UID) based patient data access system. Patients get the basic health care treatment regardless of their location through mobile technology. Even if, they don’t have access then they can come to any nearest centre for this technology to get general and specialized health services. Patient can avail the public health scheme or private insurance scheme. Patients may directly pay to the doctors or sectors via unified payments interface as an instant real time payment system. Doctors can join as an individual or as a team from any sector. They will get the service incentive quickly through this mode. The key actors of this model are depicted in Figure 2.
Proposing factors –These factors may be effective depending on further analysis of critical success factors of the e-PPP model which will define its sustainability.
Health care provider: Real time incentives encourage them to get involved in this electronic treatment approach. It also reduces the travel issues to reach to any rural sector on time.
Health care seeker: Patient can get basic and few specialized health services in their location which will be time efficient and cost effective for their disease condition. Scheme based facility is also applicable to specific scheme holders like Ayushman Bharat or National health protection scheme etc.
Public sector: Sector must strictly maintain the policy and should adequately maintain the basic technological infrastructure.
Private sector: Any private sector can join in this model but they should maintain the service rates that are same for all the sectors which are also accessible to the people.
Cloud based EHR system with e-PPP model: Inclusion of electronic health record system reduces the paperwork and introduces clarity as well as effectiveness in e-PPP model16.
This model motivates more doctors and paramedical staff to get engaged in rural area for the betterment of healthcare as well as their own career growth. The advantages of proposing e-PPP model in rural health care are mainly improvement of rural healthcare services, initiation of high-quality diagnosis and laboratory services regardless of patient-doctor location. This will also open an opportunity for rural area’s government doctors for financial incentives and further career growth through online treatment and feedback system to spread their services endlessly.
It is believed that this approach may overcome the absenteeism issues to provide effective health services continuously. It will help the overall health care system to flourish and development of digital health care initiatives for providing health care coverage to all. With the beneficial projection, this proposed e-PPP model has to overcome several challenges like data security, data access through patient card, lack of knowledge regarding online payment facility to large rural population etc. This model must attain the critical success factor and monitor the illegal or unethical activities to sustain in rural health care ecosystem.
This study suggests that e-PPP model may address the problem of absenteeism and also improve the mode of rural healthcare services. Considering the different aspects, online approach may improve their financial requisite as well as health care seeker gets better health services in remote settings. People from extremely rural areas will avail primary health care facility from specialized health care providers also via tele/m-health services. This study also recommends further survey and development of critical success factors to draw an impactful conclusion which will emphasize on introduction of e-PPP model in rural health care ecosystem in India.
References:
- Pandey, P., Sehgal, A.R., Riboud, M., Levine, D. and Goyal, M., 2007. Informing resource-poor populations and the delivery of entitled health and social services in rural India: a cluster randomized controlled trial. Jama, 298(16), pp.1867-1875.
- Dussault, G. and Franceschini, M.C., 2006. Not enough there, too many here: understanding geographical imbalances in the distribution of the health workforce. Human resources for health, 4(1), p.12.
- Banerjee, A., Deaton, A. and Duflo, E., 2004. Wealth, health, and health services in rural Rajasthan. American Economic Review, 94(2), pp.326-330.
- Banerjee, A.V., Duflo, E. and Glennerster, R., 2008. Putting a band-aid on a corpse: incentives for nurses in the Indian public health care system. Journal of the European Economic Association, 6(2-3), pp.487-500.
- National Sample Survey Organisation (2015). Key indicators of social consumption in India health, NSS 71st round (January to June, 2014).
- Das, J., Holla, A., Das, V., Mohanan, M., Tabak, D. and Chan, B., 2012. In urban and rural India, a standardized patient study showed low levels of provider training and huge quality gaps. Health affairs, 31(12), pp.2774-2784.
- Holla, A., Das, J., Mohpal, A. and Muralidharan, K., 2015. Quality and Accountability in Healthcare Delivery: Audit Evidence from Primary Care Providers in India(No. id: 7219).
- Asaria, M., Mazumdar, S., Chowdhury, S., Mazumdar, P., Mukhopadhyay, A. and Gupta, I., 2019. Socioeconomic inequality in life expectancy in India. BMJ global health, 4(3), p.e001445.
- ET Report, Literacy rate at 71% in rural India, 86% in urban: Survey by NSSO (2015) //economictimes.indiatimes.com/articleshow/47886609.cms?utm_source=contentofinterest&utm_medium=text&utm_campaign=cppst
- Planning Commission of India. High level expert group report on universal health coverage for India.2011
- Ministry of Health and family welfare, GoI. 2016. http://www.mohfw.nic.in.
- IOSR Journal of Nursing and Health Science (IOSR-JNHS) e- ISSN: 2320–1959.p- ISSN: 2320–1940 Volume 7, Issue 4 Ver. VIII (Jul.-Aug. 2018), PP 25-33
- Virani, A. and Ramesh, M., 2019. 5. How neglecting policy mechanisms can lead to policy failure: insights from public–private partnerships in India’s health sector. Making Policies Work: First-and Second-Order Mechanisms in Policy Design, pp.76-95.
- Rao, K.D., Bhatnagar, A., Berman, P., Saran, I. and Raha, S., 2009. India’s health workforce: size, composition and distribution. India health beat, 1(3), pp.1-4.
- Fabre, A. and Straub, S., 2019. The Economic Impact of public private partnerships (PPPs) in Infrastructure, Health and Education: A Review(No. 19-986). Toulouse School of Economics (TSE).
- Anurag Dubey, Implementing EMR- Are Indian Hospitals ready? eHealth magazine March 2008. http://www.ehealth.eletsonline.com


Imon Chakraborty
PhD Research Scholar
UQ-IITD Academy of Research
Indian Institute of Technology, Delhi
Mob: 825039898
Email: imon.chakraborty@uqidar.iitd.ac.in