Comparison between First and Second Wave among critically ill Patients – Prognostic Improvement or Status Quo?
Abstract
The novel Coronavirus Disease 2019 (COVID-19) has affected the healthcare systems badly and put a massive challenge across the globe. The traditional healthcare system didn’t imagine the severity and intensity of the COVID-19 pandemic which dented the economy, personal health, and human lives. As of more than one year, the challenge still persists, to save the humans from pandemic. During first wave, the situations were different as the healthcare system was not prepared and little knowledge was available. So at that time, several experiments with treatments and management of COVID-19 patients were employed, some were successful and some failed badly. However, in second wave, the lessons learnt from the previous experiments are implemented as early care. In terms of treatment, intensive care unit admissions of the critically ill patients, procedures used, are in place, which were lacking during the first wave. Though not much differences in mortality rates are observed in second wave (rate similar to first wave), in coming days, the condition may be better with development of vaccine and rapid vaccination program across the globe.
Keywords: SARS-CoV-2, COVID-19, antiviral drugs, first wave, second wave, ICU
Introduction
The first case of novel Coronavirus Disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV2), was reported in Wuhan, China, in December 2019. Since then, a total of 133,552,774 cases are recorded globally, with 2.89 million death so far (1, 2) and the counting is increasing day by day. The actual number of deaths due to COVID‑19 may be likely to be higher than the number of confirmed deaths, which could be due to limited testing and problems associated with the attribution of the cause of death (3). The entire world faced the lockdown during first wave and disconnected from each other, with merely virtually connected. The common public and the healthcare professional, including doctors, nursing, and paramedical staff, lost their lives, saving the patient’s life and fighting against the pandemic. India is no behind the rest of the world (4).
Coronaviruses, a group pf viruses, was named due to presence of crown-like spikes on surface and constitute four groups namely alpha, beta, gamma, and delta. The common human coronaviruses include 229E (alpha coronavirus), NL63 (alpha coronavirus), OC43 (beta coronavirus), and HKU1 (beta coronavirus). The other human coronaviruses include MERS-CoV (the beta coronavirus causing Middle East Respiratory Syndrome, or MERS), SARS-CoV (the beta coronavirus causing severe acute respiratory syndrome, or SARS), and SARS-CoV-2 (the novel coronavirus causing COVID-19) (5). Sometimes, the infected animals with coronaviruses provide a medium to evolve in a new human coronavirus and examples include SARS-CoV, 2019-nCoV, and MERS-CoV (5).
All virus mutate and SARS-CoV2 is no exception. Through mutation viruses constantly change over time. Due to wide circulation of virus in a population and causing infection, the virus has more opportunities to spread and replicate itself to undergo changes (6). As per research, the mutation rate of SARS-CoV-2 is estimated as 1-2 mutations per month (7). The mutation continued throughout the global crisis and currently multiple SARS-CoV-2 variants are circulating globally. The virus mutated drastically and accumulated in short span of time and causing global concern (8). There are many new SARS-CoV-2 variants with increased transmissibility and causing much higher severity of diseases than before (9). Centers for disease control and prevention identified the following variants which can spread more easily and infect quickly than other variants, and are of much concerns (10):
- 1.1.7: The variant was first identified in the US in December 2020, however, was initially detected in the UK.
- 1.351: The variant was first identified in the US at the end of January 2021, however, was initially detected in South Africa in December 2020.
- 1: The variant was first detected in the US in January 2021, however, was initially identified in travelers from Brazil tested during routine screening at an airport in Japan, in early January.
- 1.427 and B.1.429: The two variants were first identified in California in February 2021 and were classified as variants of concerns in March 2021.
COVID-19, a global pandemic now,is a serious health threat and many countries have witnessed two wave form (11).In India, COVID-19 was detected in late January 2020 and as a precautionary measure, lockdown was imposed to save 1.37 billion citizens from the infection in March 2020 (12). India witnessed the first COVID-19 wave of infections in August 2020 that peaked from September to October 2020. Now the severity and intensity of the virus can be understand by the fact that it took around 32 days for the cases to rise from 18000 to 50000 in first wave but it took only half time (17 days) for the cases to rise from 18377 to 50518 in March 2021 in the second wave as depicted in Figure (12, 13)
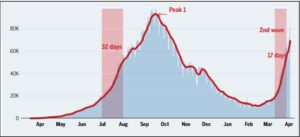
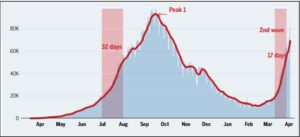
Picture Source: Times of India; 29 March 2021
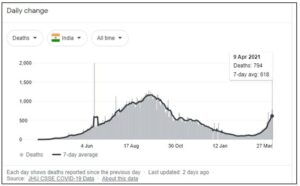
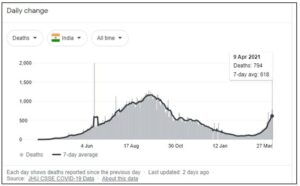
As of now, by 09 April 2021, India witnessed a total of 13.2 million cases of COVID-19 infection with 168 thousand deaths reported and increasing at a higher pace now than before (14). The most common clinical symptoms in the first wave included fever, fatigue, dry cough, myalgia, dyspnea, anorexia, and sputum production. The clinical signs and symptoms in first, as well as second wave include fever, dyspnea, cough, pneumonia, cough and most relevant comorbidities reported in patients with cardiovascular diseases, type 2 diabetes mellitus, and chronic neurological diseases (15). The current data for India is depicted below:
Treatment and Management of COVID-19 Patients
In the beginning, many countries and healthcare systems, unaware of the pandemic and limited information about the intensity of COVID-19, had confusion in efforts and treatments that led to controversial decisions about the resources, testing, and treatment (16). However, the situation improved somewhat, scientists had tried and tested various treatment to tackle the issue and were also succeeded to develop the vaccine. The strategies which were used for to manage the infection included non-pharmacological interventions (social distancing, personal protective equipment, testing and contact tracing) and pharmacological interventions (use of anti-viral therapies, other optional therapies, immune-boosters etc.) (17, 18).
Anti-viral Therapies
The most tried and tested anti-viral treatment include treatment with lopinavir/ritonavir, remdesivir, and favipiravir.
- Lopinavir/ritonavir (available in oral and liquid formulation) can also be tried in combination with interferon alpha or ribavirin, estimated to reduce replication by 50% in MERS corona virus. The adult dose is 400/100 mg per oral (PO) Q12H whereas pediatric dose varies from 12 mg/kg to 400 mg according to body weight.
- Remdesivir is one of the mostly used ant-viral used to treat the COVID-19 infection and various clinical studies were conducted to evaluate its efficacy and safety. Remdesivir has reported in-vitro activity against SARS-CoV-2 and also used against Ebola virus and found to reduce pulmonary pathology in in-vitro studies, however, hepatotoxicity was also observed (19, 20, 21). The adult dose is 200 mg intravenous (IV) on Day 1(loading dose) followed by 100 mg IV once daily (OD) for9 days, whereas pediatric dose include 5 mg/kg IV on Day 1, then 2.5 mg/kg IV Q24H in children ˂40 kg.
- Favipiravir, originally designed for influenza, is an emerging candidate in the management of COVID-19 (22). Primarily used in China and Japan, it is also garnering in India, Russia, Ukraine, Uzbekistan, Moldova, and Kazakhstan, along with UAE (22). The treatment dose is 1600 mg twice daily on Day 1, followed by 600 mg twice daily for 7 to 14 days.
Other Therapies
Other treatments used for the management of COVID-19 are provided below:
- Chloroquine or hydroxychloroquine (CQ/HCQ), though used, but no conclusive evidence established against COVID-19 (23). Better tolerability and lower incidence of toxicity were observed with use of HCQ. The treatment dose is 400 mg per oral every 12 hours on Day 1, followed by 400 mg OD. Pediatric dose include 6.5 mg/kg on Day 1 then 3.25 mg/kg Q12H for 4 days.
- Azithromycin, used with HCQ is reported to have a faster reduction in viral carriage, however, current resources are not adequate to support the use of this combination(24, 25). The treatment dose is 500 mg OD for 5 days
- Interferons (IFN-α2a, IFN- α2b or IFN-β1a) impair the antiviral adaptive type 1 T‑helper cell, however, in-vitro effects hasn’t been fully established.
- Ascorbic acidhas limited evidence suggesting that it could be beneficial in animal models of corona virus.
The other tested anti-viral medicines (oseltamivir, ganciclovir, ribavirin, favipiravir, nelfinavir, arbidol and remdesivir) with combination of CQ may be effective for COVID-19 treatment.
Who all needs intensive-care unit (ICU) admission in COVID-19
There are various factors which provide the indication for the requirement of ICU admission for COVID-19 patients. Not all COVID-19 patients require admission in ICU but there are crucial situations that lead to admission in ICU. To characterize those, there should be a uniform criterion for admission to the ICU (26). The critical conditions which require admission to ICU involve (26):
- Aged patients ≥ 65 years,
- Patients with comorbidities like hypertension, diabetes, chronic obstructive pulmonary disease (COPD), chronic kidney disease (CKD), and malignant tumors
- Patients with critical respiratory diseases
- Patients requiring frequent monitoring of the symptoms
However, patients with more than two comorbidities have escalated risks of ICU admission than those with one or no comorbidities (26, 27). So, early recognition of such patients is most important to be benefitted from ICU admission.
Role of prophylaxis in COVID-19 patients
Due to the greatly varied incidence of COVID-19 pandemic among different countries, it raises a question if the nations with a lower incidence of COVID-19 share any medical commonalities which could suggest the reason for low incidence and prophylactic treatments for other nations with high incidence rate. One such example is use of ivermectin, African countries which has the ability to inhibit SARS-CoV-2 replication, and may likely leads to lower infection rates (28).Ivermectin, as aprophylactic treatment against parasitic infections is most common in Africa, may show a correlation between prophylaxis and low incidence of COVID-19 in some countries (28). So prophylaxis plays a major role in reducing the incidence and transmission, thereby effectively slowing the spread of the disease until safe, highly efficacious vaccine is available. However, as per a review article, the use of existing molecules being evaluated in randomized clinical trials to identify successful prophylaxis against COVID-19 is yet to be established (29).
Major difference in ICU admission during first and second wave
During first wave, there was enormous admission of COVID-19 patients in ICUs, necessitating invasive mechanical ventilation, led saturation of ICUs. This exposed the specificities including necessity of deep sedation and neuro muscular blockade, increase risk of thrombotic and hemorrhagic events (30, 31) and the lengthy duration of mechanical ventilation (32) with high rate of delirium in COVID-19 patients (33). During the first wave of COVID-19, various clinical trials showed the benefits of early use of glucocorticoids in critically ill COVID-19 patients admitted in ICUs (34, 35).
During the first wave of COVID-19, many hits and trials methods were used to manage the pandemic, some were successful and some failed miserably. So the lessons and skills gained during the first wave will certainly going to help in managing the second wave of COVID-19. Researches are conducted to gain the information by comparing the features of patents, age groups, ICU treatments, and comorbidities in first and second wave, however, no major differences were noted. In second wave, the proportion of patients receiving invasive mechanical ventilation reduced and so were the incidence of thrombotic events, which could be due to early administration of glucocorticoids (36). However, there was no difference in ICU mortality and duration of ICU stay. The lower incidence of thrombotic events reported during the second wave is likely inherent to the increased intensity of thromboprophylaxis (36). Similar results for the mortality and other parameters were reported in another study conducted (37).
As far as treatment is concerned, various lessons were learned from the first wave and implements during the second wave to manage the COVID-19 patients in a better way. In first wave around 12% patients received glucocorticoids and 57% patients received intermediate or full-dose thromboprophylaxis. However, in second wave, all patient admitted received early glucocorticoids and intermediate or full-dose thromboprophylaxis that resulted in the lower rates of patients requiring invasive mechanical ventilation and lower incidence of thrombotic events (36).
Another study that evaluated the smoking and alcohol consumption revealed that smoking and alcohol consumption rate was higher in patients during second wave (13.2% and 7.3%, respectively) compared with first wave (4.9%). However, the signs and symptoms in both waves were reported as similar (fever, dyspnea, pneumonia, and cough). Patients in second wave were reported to have high incidence of vomiting and abdominal pain and less incidence of cough and chills compared with patients in the first wave. High frequency of pregnant women in second wave is noteworthy. Compared with the first wave, higher percentage of patients in second wave received treatment with corticosteroids and anticoagulants; only 4.2% patients required invasive mechanical ventilation whereas in first wave it was 13.2% patients (15) which are establishing the facts as discussed above.
Conclusion
Since its reporting to as a cluster of disease in China in December 2019 it has spread to all continents, reaching around more than 200 countries, which made WHO declare it as a pandemic. The hit and trials were tested during the first wave made some conclusions to use the best practice and those were implemented in the second wave. However, there is no difference observed in the mortality rate in first and second wave but patients admitted during second wave less likely require invasive mechanical ventilation. A combination of antiviral drugs with hydroxyl chloroquine and azithromycin (with the consultation of medical practitioner) may be the best option to treat the patients, depending on the patient’s conditions and symptoms. The lower rate of thrombotic events observed during the second wave is likely inherent to the increased intensity of thromboprophylaxis. The research and learnings from the past are continuing and warrants more robust approach as the threat still exists.