Viral hepatitis in dentistry has become a major health concern for dental health care workers.They should be vaccinated against hepatitis B.
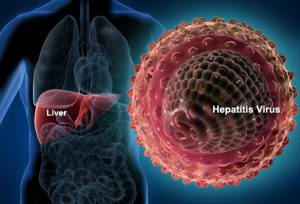 Viral hepatitis is now widely recognized as a silent epidemic worldwide. It is the major contributor towards liver cirrhosis and liver carcinoma. In a dental office, infections can be expedited through several routes, including direct or indirect contact with blood, oral fluids, droplet splatter, aerosols, etc.
Viral hepatitis is now widely recognized as a silent epidemic worldwide. It is the major contributor towards liver cirrhosis and liver carcinoma. In a dental office, infections can be expedited through several routes, including direct or indirect contact with blood, oral fluids, droplet splatter, aerosols, etc.
The presence of HCV-RNA in saliva provides a biological basis for saliva as a possible source of HCV infection, although it does not necessarily imply transmission. Lock and co-workers (2006)demonstrate a contamination with HCV-RNA of aconsiderable portion of tooth brushes used by hepatitis C patients. Dentists are in a high risk of contracting this disease due to the procedures and instruments of dental treatment.
Dentists are in a high risk of contracting this disease:
Dentists are among the highest risk of exposure of Hepatitis B virus. Reusing local anaesthetics syringes following recapping, and cleaning instruments are recognised to be the two most potential and contributing causes  of needle stick injuries in dental students and dental hygienists. Unvaccinated dentists are five times more likely to be infected than vaccinated dentists. Dental professionals are exposed to a wide variety of microorganisms in the blood and saliva of the patients.
of needle stick injuries in dental students and dental hygienists. Unvaccinated dentists are five times more likely to be infected than vaccinated dentists. Dental professionals are exposed to a wide variety of microorganisms in the blood and saliva of the patients.
Patients with liver disorders are of significant interest to the dentist because liver plays a vital role in metabolic function, including the secretion of bile needed to fat absorption, conversion of sugar to glycogen, excretion of bilirubin, a waste product of haemoglobin metabolism. Impairment of liver function can lead to abnormalities of the metabolism of amino acid, protein, carbohydrates and lipid. Many biochemical functions performed by the liver, such as synthesis of coagulation factors and drug metabolism, may be adversely affected.
Standard precautions for the minimum infection:
Standard precautions are the minimum infection prevention practices that apply to all the patient care, regardless of suspected or confirmed infection status of the patient, in any setting where health care is delivered. These practices are designed to both protect DHP (Dental Health Providers) and prevent DHP from spreading infections among patients. Standard precautions include:
1. Hand hygiene
2. Use of personal protective equipment (e.g., gloves, masks, eyewear)
3. Respiratory hygiene/ cough etiquette.
4. Sharps safety (engineering and work practice controls)
5. Safe injection practices (i.e., aseptic technique for parenteral medications).
6. Sterile instruments and devices.
7. Clean and disinfected environmental surfaces.
Guidelines for treating hepatitis patient:
 A. No dental treatment other than urgent care should be rendered for a patient with acute viral hepatitis
A. No dental treatment other than urgent care should be rendered for a patient with acute viral hepatitis
1. Hepatitis B is of primary concern to the dentist. Individuals still carry the virus up to 3 months after the symptoms have disappeared, so any patient with a recent history of hepatitis B should be treated for dental emergency problems only.
2. For patient with a past history of hepatitis, consult the physician to determine the type of hepatitis, course and length of the disease, mode of transmission, and any chronic liver disease or viral carrier state
3. For recovered HAV or HEV, perform routine periodontal care.
4. For recovered HBV and HDV, consult with the physician and order HBsAg and HBs laboratory tests.
5. If HBsAg and anti-HBs tests are negative but HBV is suspected, order another HBs determination.
6. Patients who are HBsAg positive are probably infective (chronic carriers); the degree of infectivity is measured by an HBsAg determination.
7. Patients who are anti-HBs positive may be treated routinely.
8. Patients who are HBsAg negative may be treated routinely.
B.If a patient with active hepatitis, positive-HBsAg (HBV carrier) status, or positive HCV status requires emergency treatment, use the following precautions
1. Consult the patient’s physician regarding status
2. If bleeding is likely during or after treatment, measure prothrombin time (PT) and bleeding time. Hepatitis may alter coagulation; change treatment accordingly
3. All personnel in clinical contact with the patient should use full barrier technique, including masks, gloves, glasses or eye shields, and disposable gowns
4. Use as many disposables covers as possible, covering light handles, drawer handles, and bracket trays. Headrest covers should also be used
5. All disposable items (e.g., gauze, floss, saliva ejectors, masks, gowns, gloves) should be placed in a lined wastebasket. After treatment, these items and all disposable covers should be bagged, labelled, and disposed of, following proper guidelines for bio-hazardous waste
6. Aseptic techniques should be followed at all times. Minimize aerosol production by not using ultrasonic instrumentation, air syringe, or high-speed handpieces. Remember that saliva contains a distillate of the virus. Pre-rinsing with chlorhexidine gluconate for 30 s is highly recommended
7. When the procedure is complete, all equipment’s should be scrubbed and sterilized. If an item cannot be sterilized or disposed of, it should not be used.
8. All working surfaces and environmental surfaces should be wiped with 2% activated glutaraldehyde (Cidex).
Recommendations for dentist:
Dental health care workers, should be concerned primarily with HBV, HCV and HDV, as occupational exposure to these pathogens places them at risk of developing acute or chronic infections. Vaccines and immune globulins are available and effective in protecting against infections with HAV, HBV and HDV, but not HCV. Dentists should become knowledgeable about viral hepatitis. They should be vaccinated against hepatitis B. Adherence to infection control measures will help prevent occupational transmission of all bloodborne pathogens, including hepatitis viruses.
1. Get vaccinated against Hepatitis B & get your Anti HBs titres checked.
2. Treat all patients as potentially infectious.
3. Follow safe injection practices and infection control protocol.
4. Don’t ignore if any NSI occur.
5. Handle the sharps with extra caution.
6. Spread awareness about Viral Hepatitis.

Dr Sabin Syed
Program Coordinator – ECHO & PRAKASH
Institute of Liver and Biliary Sciences-New Delhi
Mob: 9911071707
(Valuable Contribution – Team PRAKASH)